In modern clinical monitoring, if the ECG is the heart’s business card, the Capnography waveform is the patient’s comprehensive digital projection. While pulse oximetry (SpO2) measures the result of oxygenation—often with a significant time lag—Capnography measures the process of breathing in real-time.
By integrating ventilation, perfusion, and metabolism, capnography transforms clinical observations into actionable data.
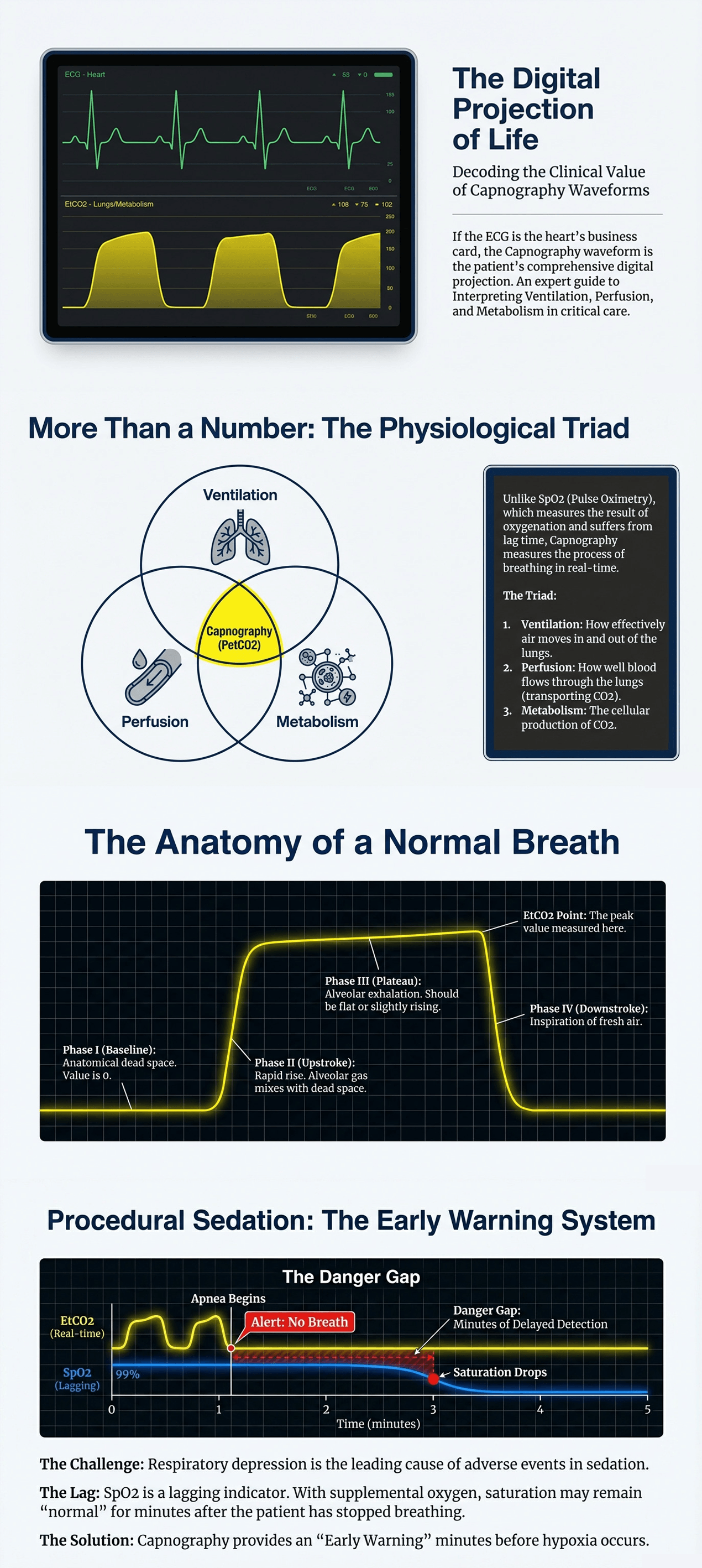
Capnography (PetCO2) is a unique window into the body's internal state because it sits at the intersection of three vital systems:
Ventilation: Reflects how effectively air moves in and out of the lungs.
Perfusion: Indicates how well blood flows through the lungs to transport CO2.
Metabolism: Monitors the rate of cellular CO2 production.
Clinical mastery begins with recognizing the normal capnogram, which consists of four distinct phases:
Phase I (Baseline): Exhalation of anatomical dead space (contains no CO2); the baseline should remain at zero.
Phase II (Upstroke): A rapid rise as alveolar gas mixes with dead space gas.
Phase III (Alveolar Plateau): The peak of this phase represents the actual EtCO2 value.
Phase IV (Downstroke): The rapid onset of inspiration, bringing the curve back to zero.
Respiratory depression is the primary risk during sedation. In patients receiving supplemental oxygen, SpO2 may stay normal for several minutes even after breathing has stopped.
Early Detection: Capnography identifies apnea or hypoventilation instantly, providing a vital warning window before hypoxia occurs.
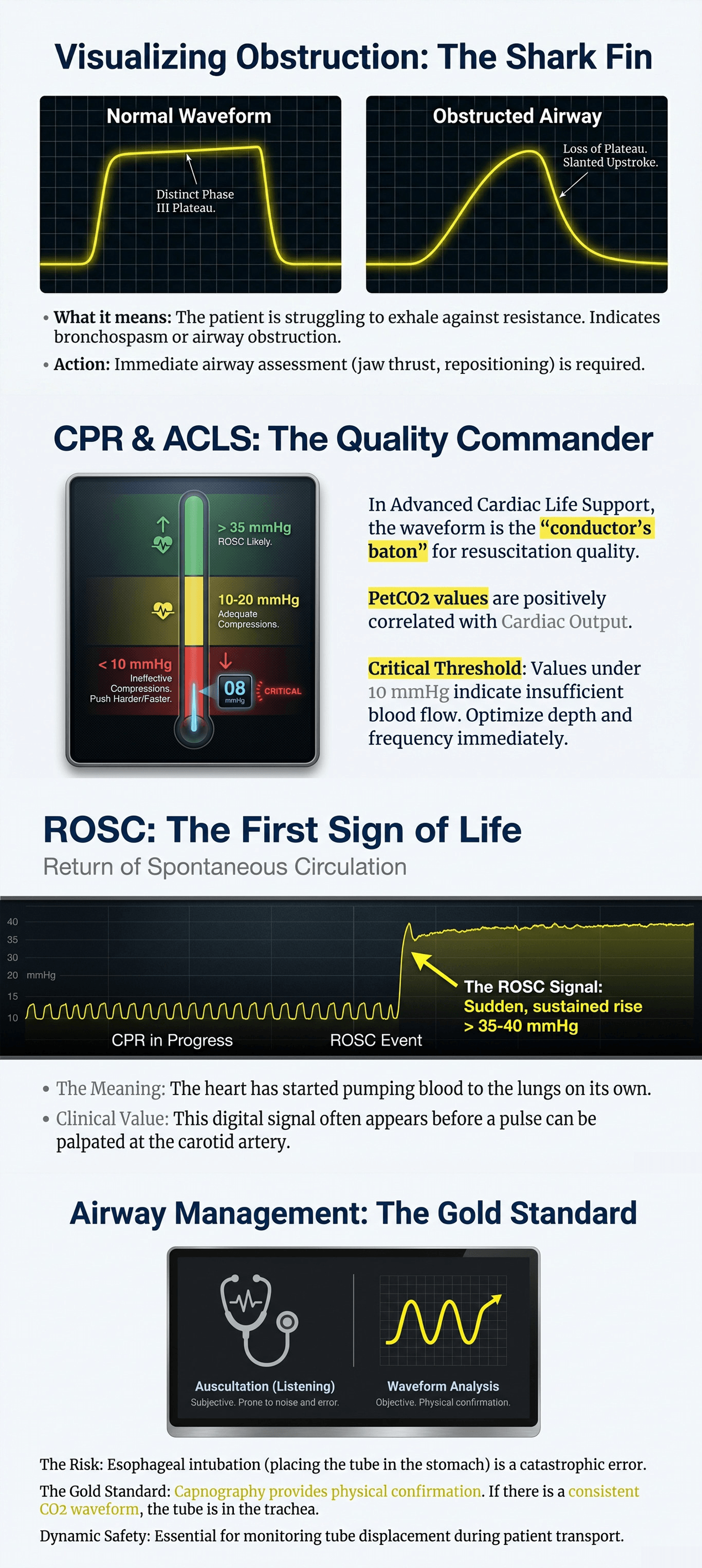
In Advanced Cardiac Life Support, EtCO2 is the most reliable physiological indicator of chest compression quality.
Compression Feedback: Values below 10 mmHg signal the need to improve compression depth or rate.
Predicting ROSC: A sudden, sustained jump in EtCO2 (typically to 35-40 mmHg) is often the first sign of Return of Spontaneous Circulation (ROSC).
Relying on lung auscultation to confirm tube placement is subjective and prone to error.
Physical Confirmation: A sustained CO2 waveform is the only objective evidence of tracheal intubation. A flatline or diminishing "bumps" indicates esophageal placement—a potentially fatal error.
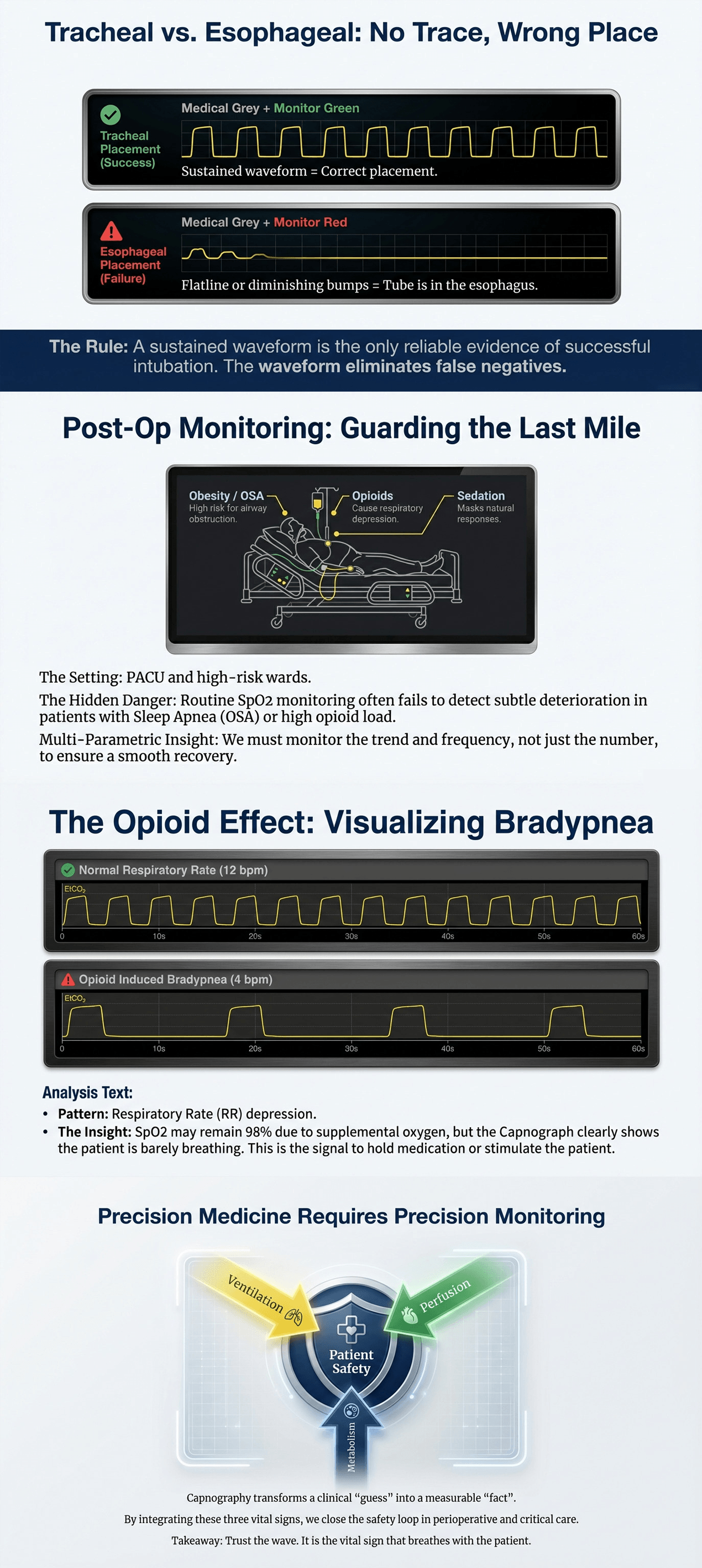
For patients with obesity, Sleep Apnea (OSA), or those on opioid analgesics, the risk of "silent" respiratory failure is high.
Continuous Vigilance: Monitoring the trend and frequency of the waveform allows staff to detect subtle deterioration that routine spot-checks might miss.
The shape of the wave is as critical as the number. A slanted upstroke with a disappearing plateau creates a "Shark Fin" appearance.
Clinical Significance: This indicates obstructive exhalation, typically seen in bronchospasm or airway obstruction, requiring immediate intervention.
Precision medicine requires precision monitoring. Capnography bridges the gap between ventilation and circulation, providing a real-time safety net for patients. By moving beyond simple numbers and trusting the waveform, clinicians can achieve the highest standard of patient safety.