End-tidal carbon dioxide (ETCO₂) is more than a respiratory monitoring tool—it serves as a dynamic window into the patient’s overall physiological status. By reflecting alveolar ventilation and circulatory perfusion in real time, ETCO₂ provides critical insights in anesthesia, critical care, and emergency settings, helping healthcare professionals make timely and informed decisions.
Understanding the key clinical factors that influence ETCO₂ is essential for accurate interpretation of both values and waveforms, enhancing the precision of patient monitoring.
Blood circulation directly affects CO₂ transport to the alveoli, making ETCO₂ closely linked to perfusion status.
Typical observations:
ETCO₂ may drop significantly, while oxygen saturation and ventilation remain normal
Waveforms usually remain stable
Clinical insights and strategies:
When ETCO₂ decreases abruptly, assess blood pressure, heart rate, skin temperature, urine output, and lactate levels
During anesthesia, consider sedation depth and medication timing for interpretation
In ICU settings, focus on ETCO₂ trends rather than single readings, using them as an early indicator of perfusion changes
The patient’s respiratory rhythm, depth, and regularity can significantly influence ETCO₂ waveforms and numerical values.
Cause: Reduced alveolar ventilation, decreasing CO₂ elimination
Strategy: Observe for short, flattened waveforms and shorter cycles; consider arterial blood gas correlation; focus on trends in anxious or painful patients
Cause: Extended exhalation allows CO₂ to be fully expelled → ETCO₂ values rise
Strategy: Interpret alongside respiratory rate and sedation status; avoid misjudging hypoventilation or respiratory compromise
Cause: Variable tidal volumes or intermittent sigh-like breaths
Strategy: Focus on trends; fluctuations are normal during anesthesia recovery or in patients with altered consciousness; prioritize waveform analysis over absolute values
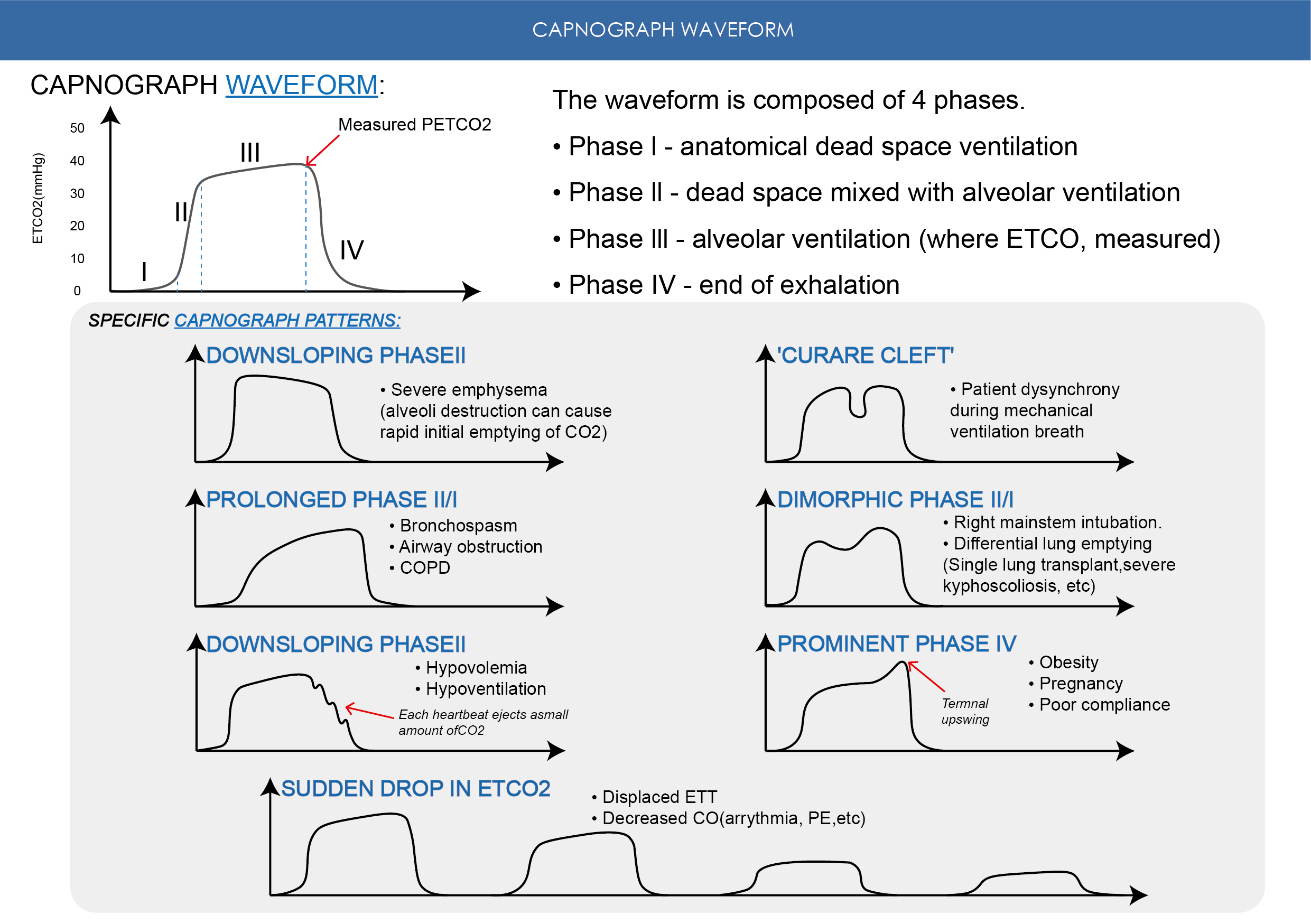
Airway obstruction, bronchospasm, or uneven alveolar ventilation can all affect ETCO₂ waveforms and values.
Impact: Exhalation difficulty produces a “shark fin” waveform; ETCO₂ may be elevated or delayed
Strategy: Monitor end-exhalation waveform changes; assess airway resistance via compliance and auscultation; waveform patterns are more reliable than numerical values
Impact: Inconsistent CO₂ elimination from different lung regions can lead to falsely high or low ETCO₂ readings
Strategy: Focus on trends rather than absolute values; consider arterial blood gas “PaCO₂ – ETCO₂ difference”; adjust ventilation strategies based on lung compliance and waveform patterns
The key to ETCO₂ monitoring lies in trends and waveforms, not isolated readings. Circulatory perfusion, breathing patterns, and airway conditions all leave detectable signatures in ETCO₂. By understanding these factors, healthcare professionals can:
Accurately interpret ETCO₂ changes
Avoid misattributing normal physiological fluctuations to device errors
Use ETCO₂ as a comprehensive indicator of ventilation, perfusion, and patient condition trends
With our ETCO₂ monitoring devices, clinicians can capture subtle changes in patient respiration and circulation in real time, providing reliable support for clinical decision-making and fulfilling the ultimate promise of “monitoring respiration, understanding physiological status.”