End-Tidal carbon dioxide has become a standard monitoring tool for airway management. Through monitoring EtCO2, it can avoid some related deaths effectively caused by airway
management. Not only in airway management, EtCO2 can also reflect the patient's metabolic parameters (CO2 produced by the body) and respiratory parameters (dead space, minute ventilation).
Attention for clinical uses:
1. The value of EtCO2
2. The changes of EtCO2 under the support of other parameters (i.e. settings of tidal volume and trend of ventilation)
3. The waveform of EtCO2
4. The factors and limitations affecting EtCO2
Before knowing the further application of EtCO2, we need to know the connection of arterial blood, EtCO2 and dead space (physiological dead space and mechanical dead space)
End-tidal carbon dioxide is the concentration of carbon dioxide in the gas at the end of exhalation. The measured value at this time is the similar to the value of alveolar carbon dioxide, and at this time the pressure of carbon dioxide is roughly the same as PACO2. However, when actually measured, the value of PACO2 will be slightly higher than end tidal carbon dioxide by 3-10 mmHg. It is mainly because the dead space will not participate in the calculation of carbon dioxide when measuring. For example, physiological dead space include anatomical dead space and alveolar dead space. The anatomical dead space refers to the passage of gas into trachea or bronchi which don’t participate in gas exchange during each breath. Alveolar dead space refers to dysfunctional alveolar, which can not convert carbon dioxide. It can be seen that the influencing factors for the measurement of end-tidal carbon dioxide are closely related to the dead space volume.
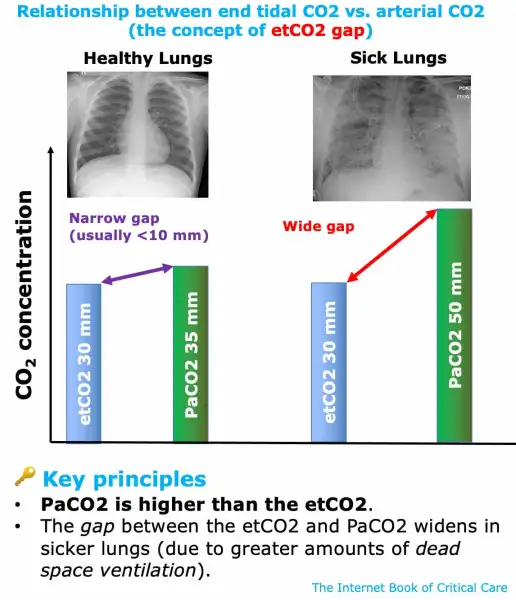
In clinical practice, most doctors want to observe and predict the exact situation of PaCO2 through the value of EtCO2. However, this application depends on whether the patient's own ventilation function is good, that is to say, if the patients have lung disease. Many studies have shown that when comparing EtCO2 and PaCO2 for patients without lung diseases, PaCO2 is often slightly higher by 3~8mmHg. But for patients with lung disease, the difference between EtCO2 and PaCO2 will increase substantially. The change of the ventilation volume and the setting of the ventilator can lead to an increase in the dead space volume of the patient, so that the difference between EtCO2 and PaCO2 can be enlarged. However, we can still observe the change of PaCO2 in real time by observing the end-tidal capnogram after the patient's condition is stable. Even if there is a large gap between the two values, the correlation still exists, and the trend of the two changes tends to be consistent.